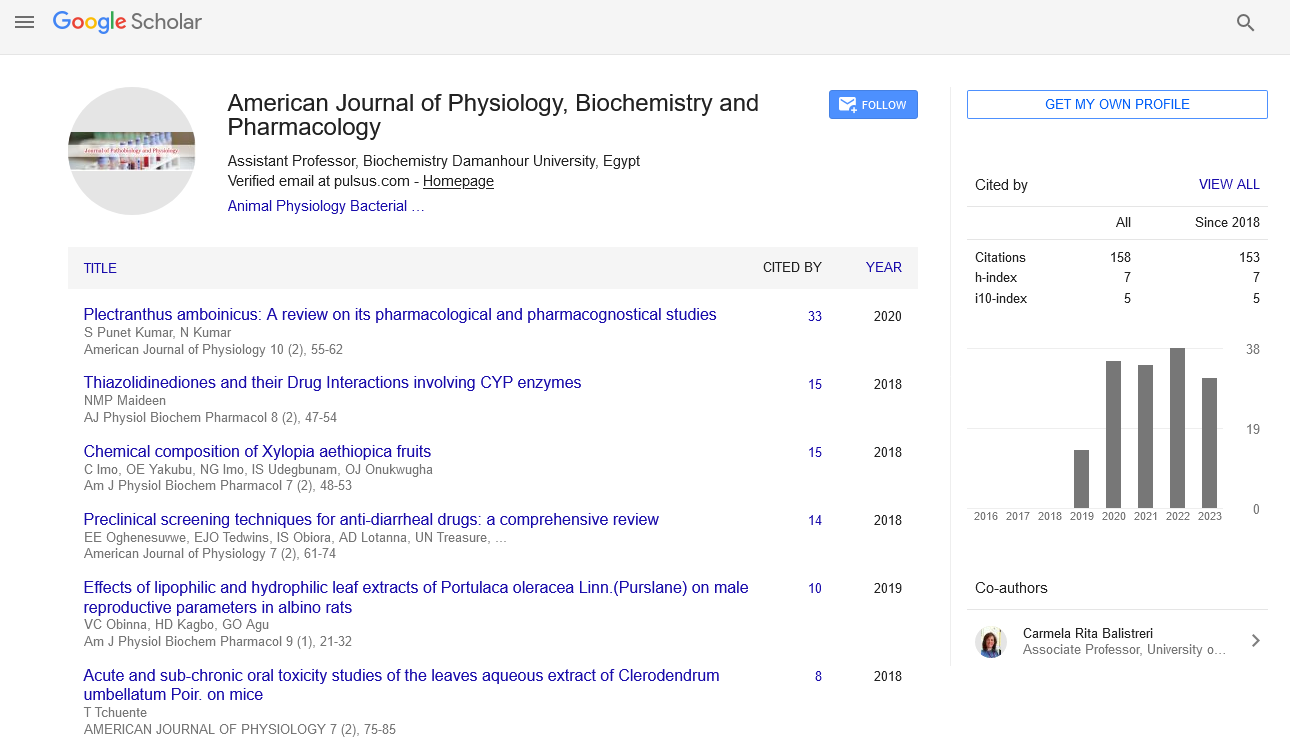
Commentary - American Journal of Physiology, Biochemistry and Pharmacology (2022)
Physiological Response of Human Brain Death and Use of Organ Transplantation
Xiaooli Zhang*Xiaooli Zhang, Department of Pharmacology, Northwest University, Shaanxi, China, Email: xiaolizang@gmail.com
Received: 24-Aug-2022, Manuscript No. AJPBP-22-72692; Editor assigned: 29-Aug-2022, Pre QC No. AJPBP-22-72692 (PQ); Reviewed: 12-Sep-2022, QC No. AJPBP-22-72692; Revised: 19-Sep-2022, Manuscript No. AJPBP-22-72692 (R); Published: 26-Sep-2022
Description
Physiology is a branch of biology that focuses on how organ systems, specific organs, cells, and biomolecules perform the chemical and physical processes necessary for a living system to function. The scientific study of a biological organism works and how its mechanisms work is called physiology. The heart and circulatory system are two examples of organs that are researched in terms of their overall function in relation to cellular and molecular biological changes.
Organ physiology encompasses research on the heart and circulatory system in the overall function of the organ is examined in relation to cellular and molecular biological changes. The transplanted organs are sourced from deceased brain-dead donors both inside the Euro transplant zone. An organ is removed from one body and implanted in the body of the recipient during an organ transplant operation to replace a damaged or absent organ. Successful organ transplants have been performed on the heart, kidneys, liver, lungs, pancreas, intestine, thymus, and uterine. Tissues include corneae, skin, heart valves, nerves, and veins. The most often transplanted organs globally are the kidneys, the liver, and lastly by the heart. The common transplanted tissues are musculoskeletal and corneal grafts and which outweigh organ transplants by a factor.
Brain death is a tragic physiological occurrence that causes other organs to function significantly differently. A catastrophic occurrence such as brain death causes severe systemic disturbances which are involved by haemodynamic instability, inflammatory, hormonal, metabolic, and haematological diseases. It is widely established by kidney grafts obtained from living donors are both related to recipients and those who are not perform significantly better than those obtained from deceased donors in terms of delayed graft function, acute rejection, and graft survival. The emphasis has recently turned from recipient to donor and the events taking place at the time of brain death since there is a considerable difference between the short and long term survival of kidneys from living and deceased donors. After deaths have been determined by the loss of circulation, a number of tissues can still be obtained for transplantation. The circulation can be maintained for hours or days after death has been decided by the loss of all brain function to allow for the retrieval of organs.
The psychological issues that are mainly concerned with living organ donation include preventing psychological harm and making sure donors are fully informed and choose to donate without coercion and monitoring donor psychosocial outcomes. These issues are closely related to the things that have historically served as barriers to using organs from living donors. By inspiring the public and raising individual knowledge, responsibility from these obstacles can be overcome. Brain death has emerged as one of the main elements thought to have a substantial impact on transplant function and survival. Vast cardiovascular, respiratory, endocrine, metabolic, and haematological alterations result after brain stem death. The control of these abnormalities is essential from the organ donation is a possibility to boost the success rates of transplantation. It is advised to employ protocols to assure the best possible management of any potential heart-beating organ donors and to use target-driven therapy to help guide treatment.
Copyright: © 2022 The Authors. This is an open access article under the terms of the Creative Commons Attribution NonCommercial ShareAlike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.